
The Alliance for Pulmonary Hypertension (AfPH) places a strong emphasis on the sharing of knowledge and best practices as a means to empower patients and family members and advance the understanding and treatment of pulmonary hypertension. This is the rationale behind the creation of the Pulmonary Hypertension Knowledge Sharing Platform, an open, inclusive, and dynamic space where members of the community can find and share information.
As part of its educational program for this year on April 29 the Alliance for Pulmonary Hypertension hosted a webinar with two world renowned experts in the field of surgical and interventional treatments in chronic thromboembolic pulmonary hypertension (CTEPH), a rare form of pulmonary hypertension, characterized by the presence of organized thromboembolic material (clots) and vascular remodelling. It is classified in Group IV of the current official World Health Organization (WHO) classification of pulmonary hypertension.
David Jenkins MS (London), FRCS (CTh), is Clinical Director of Surgery and Consultant Cardiothoracic Surgeon at the Royal Papworth Hospital, Cambridge, UK. He is a leading world expert in “pulmonary endaterectomy” (PEA), the surgical option of choice for patients with accessible (proximal) pulmonary artery lesions. PEA consists of a complete bilateral clearance of the pulmonary arteries down to segmental and subsegmental levels, in phases of deep hypothermic circulatory arrest, to remove all the thrombotic material. x
Prof. Hiromi Matsubara is Deputy Director of the National Hospital Organization, Okayama Medical Center, Japan. He is a pioneer and acclaimed world expert in “balloon pulmonary angioplasty”, BPA, an established treatment for selected patients with inoperable CTEPH or persistent/recurrent pulmonary hypertension after PEA. In BPA the obstructed vessels are opened or widened by using a catheter-based intervention to restore pulmonary blood flow. Four to five sessions would be required to complete the treatment depending on the individual cases. Both interventions have the potential to normalize pulmonary haemodynamics and functional capacity of patients. PEA and BPA are extremely complex, but very effective, procedures which require highly specialised skills.
During the webinar our guest speakers mentioned that they travel to share their experience and expertise with colleagues in other countries. After the event we followed up on this topic to gain insights from them into how these exchanges are organized in order to better understand their significance in shaping medical advancements.
We are deeply grateful to both David Jenkins and Hiromi Matsubara for having graciously accepted to share their experience. It is truly inspiring to see the extensive efforts they are making to enhance awareness about PEA and BPA, thus advancing healthcare around the world in the field, and paving the way for more patients to access these potentially life-saving surgical interventions.
Organisational aspects of exchanges
When it comes to organizing these exchanges, both revealed that these are typically informal, tailored to suit the dynamics of the medical team he is visiting. Over the past years, David Jenkins has traveled to at least ten medical centers across various continents. Image n°1 image below shows the different types of interactions between the surgeons at Papworth Royal Hospital and medical centres around the world. Prof. Matsubara has visited about twenty centers, mainly in East Asia and Europe. He recommends visiting his center before starting a BPA program, and, if necessary, he visits the center to do the initial cases. Image n° 2 provides the details.
Follow up contacts and activities
David Jenkins explained that these visits are not merely fleeting encounters. They often lay the groundwork for ongoing collaboration and follow-up discussions, extending beyond geographical boundaries. Through virtual meetings cases are deliberated upon, insights shared, and collective wisdom harnessed to optimize patient outcomes. In the case of Prof. Matsubara, after experiencing some BPA cases, the operators may need additional knowledge for improving their outcome. In that case he recommends revisiting his center to update their knowledge and technique.
Benefits of medical exchanges
It is important to note that the benefits of such exchanges are enormous and extend well beyond the individual institutions concerned. They contribute to the advancement of the entire medical community, driving collective progress and raising standards of care globally. As medical centers collaborate to tackle such complex surgical challenges, they contribute to the body of knowledge that shapes clinical guidelines, protocols, and training programs, ensuring that future generations of surgeons are equipped with the latest advancements and best practices.
Conclusions
In essence, exchanges between medical centers represent a cornerstone of modern healthcare, serving as catalysts for innovation, collaboration, and continuous improvement. By fostering a culture of sharing and learning, these exchanges empower surgeons to deliver the highest quality of care to patients undergoing complex surgical interventions, ultimately transforming lives and shaping the future of medicine.
IMAGE 1
Okayama Medical Center (OMC) Japan international balloon pulmonary angioplasty (BPA influence
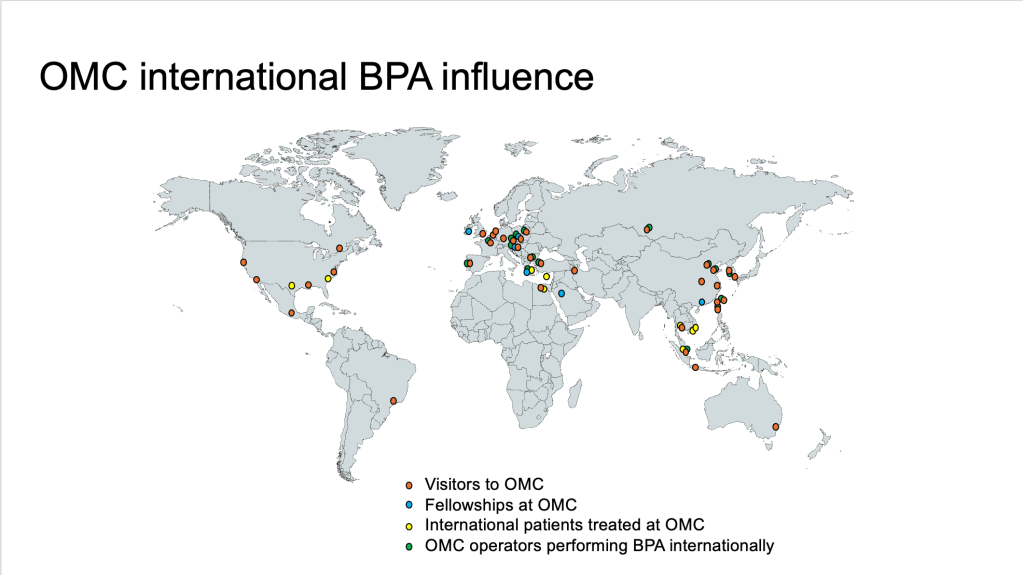
IMAGE 2
Royal Papworth Hospital (RPH) international pulmonary endarterectomy influence

THE SLIDES AND RECORDING OF THE WEBINAR ON SURGICAL INTERVENTIONS IN CHRONIC THROMBOEMBOLIC PULMONARY HYPERTENSION IS AVAILABLE AT THIS LINK

